
Research at the University of Florida has shown the value of One AC, a feed supplement consisting of L-tyrosine, niacin, and vitamin C developed by Raymond LeRoy, a biochemist from Phoenix. LeRoy theorizes that anhydrosis is caused by a depletion of dopamine in the brain.
"The available dopamine is used first by the brain, second by the cardiovascular system, and third by the sweating system," LeRoy explained. "If the horse is not producing enough dopamine to satisfy the three systems, then sweating is compromised in favor of the brain and cardiovascular system. One AC provides the necessary raw materials to compensate for the depletion, and the animal returns to the sweating function."
When the weather is particularly hot and muggy, horses often are drenched with sweat even if they are doing nothing more strenuous than grazing. They might appear to be uncomfortable, but they are actually much cooler than the horse that is standing in the shade and panting because he is not sweating.
Anhydrosis-the partial or total inability to sweat-has been recognized in horses since the early 1920s. No definite reason has been discovered as to why some horses develop the problem, which can affect all ages and breeds. Anhydrosis is most commonly seen in horses living in America's Gulf Coast states, including Florida and Louisiana, and in South Texas.
The combination of heat and humidity appears to cause the problem; heat alone is not to blame. The condition can occur just as easily in imported horses as in horses that are native to the area.
The danger in hot, humid climates is that horses that do not receive a break from the heat can become heat stressed (compromised sweating) or stop sweating completely.
"It's important to get horses out of the heat for at least a few hours every day," noted Ralph Beadle, D.V.M., Ph.D., and professor emeritus at Louisiana State University School of Veterinary Medicine. Beadle taught at LSU's Veterinary Clinical Sciences Department of Equine Medicine for 25 years before he retired in 1999.
"If you continuously stimulate the sweat-gland receptors, eventually they quit responding," Beadle noted. "We see the problem here in Louisiana when the temperature doesn't go below 70 degrees at night, plus we have the high humidity to go with it. A nonsweater shuts down altogether, while heat-stressed horses still sweat some, but not as much as we'd like to see. If temperatures drop down into the low sixties at night for several consecutive days to weeks, then we'll see them start sweating again."
Understanding Anhydrosis
Horses are designed to eliminate excess body heat and cool themselves through the evaporation of sweat. When a horse stops sweating, he tries to cool himself through a panting form of breathing. This forces cool air to move across his respiratory tract; when water evaporates from this surface, the horse is helped somewhat, but it is not an efficient method of cooling. Even at rest, the nonsweater's body temperature may rise to between 102 degrees and 103 degrees. Add exercise to this dangerous equation and the animal's temperature can reach 105 degrees to 108 degrees. Brain damage is possible when the body temperature exceeds 106 degrees.
Signs of anhydrosis include panting, rapid breathing with noticeable flaring of the nostrils; decreased energy; and sparse, dry hair coat, sometimes with scaliness or thinned hair on the face, neck, and shoulders. A veterinarian can perform a "sweat test" to see how severely a horse is affected and to determine if the horse is actually a nonsweater or is heat-stressed.
Normally, a horse will cool out after exercise within 30 minutes. If the horse's rectal temperature remains elevated for longer than this, anhydrosis should be considered.
A combination of stressors can make a horse stop sweating. "We sweat-tested a group of horses at a racetrack and examined one that was sweating fine on Friday," recalled Beadle. "He raced over the weekend and chipped an ankle. By Monday, this horse was not sweating; the combination of heat, stress, and pain threw him into it. We don't know if horses are genetically predisposed [to become nonsweaters], but we do know that environment plays a big part in it."
A horse might sweat normally, even excessively for a few days, then shut down altogether. "Some horses will stop sweating overnight," noted Gary Norwood, D.V.M., of Backstretch Surgery and Medicine in New Orleans. A former president of the American Association of Equine Practitioners, Norwood has been involved with anhydrotic horses since the mid-1970s. "It's a very puzzling problem for those of us who work in the South."
Managing anhydrosis
Because there is no cure for this frustrating and potentially dangerous condition, managing the anhydrotic horse and its environment are the only options. The obvious, though often least practical, solution is to ship the nonsweater to a cooler, less-humid climate. When this is not possible, the key is careful, observant management, particularly before the animal stops sweating completely.
Therefore:
- Restrict physical activity of affected horses during hot, humid hours; and
- Exercise horses only in the early morning or late evening.
Anhydrotic horses will attempt to find ways to cool off by seeking shade, lying in damp areas, splashing water on themselves from the trough or bucket, or standing in any available water. Some horses will take advantage of sprinkler systems set up in the pasture, but to monitor the horse better, the animal should be in a shaded area with moving air, such as in a stall equipped with a fan or, even better, a misting fan. Use of misting fans or simply running cool water on the barn roof can lower temperatures in the barn by as much as 10 degrees.
Norwood notes there are numerous anecdotal remedies that horsemen have employed to manage anhydrosis. Adding coffee grounds to the feed is one old Cajun trick that some claim is effective. Adding beer to the feed is another method that has proven helpful in some cases. "Lite" salt (a combination of regular salt and potassium chloride) also can be added to the horse's daily grain ration to help promote sweating.
When used to treat respiratory conditions, sweating is often a side effect of the drug clenbuterol. Because of this, some people have used clenbuterol to manage anhydrosis, but Norwood cautions against this. "If sweat receptors are over stimulated enough, they will actually become desensitized," Norwood said.
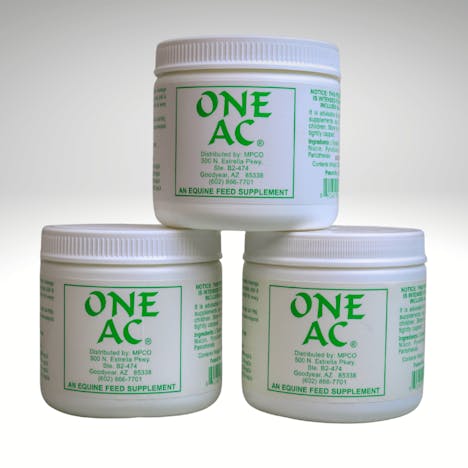
Research at the University of Florida has shown the value of One AC, a feed supplement consisting of L-tyrosine, niacin, and vitamin C developed by Raymond LeRoy, a biochemist from Phoenix. LeRoy theorizes that anhydrosis is caused by a depletion of dopamine in the brain.
"The available dopamine is used first by the brain, second by the cardiovascular system, and third by the sweating system," LeRoy explained. "If the horse is not producing enough dopamine to satisfy the three systems, then sweating is compromised in favor of the brain and cardiovascular system. One AC provides the necessary raw materials to compensate for the depletion, and the animal returns to the sweating function."
Horses generally start sweating again within ten to 14 days of starting on One AC, noted LeRoy. He stresses that horses must be taken out of training for about three weeks when initially started on the supplement to allow the system to respond properly. Reintroduced too soon, hard cardiovascular work will deplete the amount of dopamine necessary for stimulating the sweat glands. Horses can usually be put back into training after three weeks without disrupting the sweating process. Some owners keep their anhydrotic horses on One AC year-round and simply lower the dose during the cool months.
Norwood also reports that some veterinarians have successfully used methyldopa on resistant cases when they have not had luck with other treatments.
Attentive management
Norwood has found One AC to be about 30% to 70% successful in his practice. It is important to catch the horse early and start using the supplement before he totally stops sweating. In the case of a horse that has been anhydrotic in the past, you should assume he will have this problem again and put him on the supplement before the arrival of hot, humid weather.
Going into the summer months, make sure horses are at optimum health and up to date on deworming and vaccinations. Try to have horses as fit as possible coming into the hot, humid season so they will not have to train as hard during this potentially stressful time of year.
Keep horses eating and well hydrated. Oral electrolytes often are recommended and can be added to the horse's water, grain, or both. Beadle suggests giving the horse two sources of water. This can be as simple as hanging two buckets-one with plain water and the other with water and electrolytes. Hanging two buckets in the stall will easily show you if the horse is drinking the electrolyte water. In some cases, your veterinarian may recommend administering electrolytes via nasogastric tube.
What is Anhydrosis in Horses?
How Can One AC Help Non-Sweaters?











Technical Scientific Paper:
Equine Anhidrosis
Vet Clin Equine 18 (2002) 355-369
Equine anhidrosis.
Jeremy D. Hubert, BVSc, MRCVS, MSa,*,
Ralph E. Beadle, DVM, PhDa, Gary Norwood, DVMb
School of Veterinary Medicine. Department of Veterinary Clinical Sciences. Equine Health Studies Program, Louisiana State University. Baton Rouge. LA 70803.
USA b Backstretch Equine Surgery and Medicine. 539 Bonnabel BOlllevard. Metairie. LA 70005. USA
Equine anhidrosis, dry coat, and nonsweating are all terms used to describe the disease in horses characterized by the inability to sweat effec¬tively in response to appropriate stimuli. Although the epidemiology and clinical signs of the disease have largely been elucidated, anhidrosis is still widely prevalent, and methods of prevention and treatment are being sought. Initial reports date back to the 1920s, when Thoroughbreds from Australia developed this condition after being transported to Malaysia [1]. Later it was reported that such horses improved once they were removed from the tropical environment and maintained 10 to 30 days in a cooler and drier climate. [2]. This article reviews the epidemiology, proposed pathophy¬siologic mechanisms, clinical features, diagnosis, and treatment.
Epidemiology of anhidrosis
The disease commonly occurs in countries with hot, humid climates including the American Gulf Coast states. The precise prevalence of the dis¬ease is unknown; however, it has been estimated that up to 20°/c) of horses in the Miami area of Florida may be affected [3,4]. Anhidrosis was originally assumed to be associated with an acclimatization stress [2], but a survey con¬ducted in Florida in 1982 showed that more native horses were affected than imported horses [4]. Horses involved in strenuous activities were origi¬nally reported to be the most prone to develop anhidrosis [2], but this does not correlate with a study where only 7 out of 24 affected horses were performance horses [4]. Another study found that the frequency is higher in horses in training and lower in adolescent horses [3]. There is no coat color, age, sex, or breed predilection. A link between anhidrosis and high protein diets has been reported [5], but this finding was not corroborated in another study [4]. Nonpregnant mares were reported in one study to have a statistically significant higher incidence of anhidrosis [3].
Clinical signs of anhidrosis
Horses with normal thermoregulatory abilities will be able to reduce their body temperature to within normal limits in approximately 30 minutes after exercise, and the inability to cool out to normal temperatures within this time is indicative that a horse may be suffering from anhidrosis. The pre-dominant' sign of impending anhidrosis is usually tachypnea [3]. Affected horses will have increased respiratory rates at rest, while body temperature and pulse rate are variably increased when compared with those of control horses under identical conditions [2-5]. Horses showing evidence of respira¬tory distress will have respiratory rates between 60 and 120 breaths per minute [3]. Partially anhidrotic horses will breath rapidly for extended peri¬ods of time after being thermally challenged [3]. Horses with acute onset anhidrosis may demonstrate a partial or complete absence of sweating when exposed to appropriate stimuli. A decrease in the rate of sweating also indi¬cates the possibility of anhidrosis. The sweating rate will, however, depend on the intensity of exercise, duration of exercise, and ambient temperature [6]. Horses with long-standing anhidrosis may reveal dry, flaky skin, alope¬cia, lethargy, anorexia, and a decreased water intake. Areas on the body that may retain the ability to sweat include those under the mane, in the saddle . and halter areas, and in the axillary, inguinal, and perineal regions [2-5].
Thermoregulation in horses
Thermoregulation is attained by two main mechanisms in terrestrial mam¬mals; namely panting and sweating [7]. Heat dispersed via the respiratory tract in exercising horses may account for 15% to 25% of total heat loss, whereas evaporation of sweat accounts for up to 65% of their heat loss [6]. In this regard, it has been calculated that evaporation of 1 liter of sweat can dissipate the amount of heat generated in I to 2 minutes of high-intensity exercise by horses [8].
During exercise there is an initial rise in temperature, which may be advantageous for performance because it increases the rate of aerobic energy production, thereby minimizing the necessity for anaerobic energy production [9]. As work effort increases, heat production in skeletal muscle can increase more than 50 times [I 0]. This heat is derived from the conver¬. SiOll of chemical energy into mechanical work. Only 25°/r, of the metabolic energy is converted to mechanical work, with the remainder generating body heat, which must be dissipated during or after exercise [11]. A number of factors can influence the rate at which horses lose heat by the evaporation of sweat. First, the rate at which heat can be dissipated by evaporation depends upon the rate of air movement across the skin and the water vapor pressure difference between the skin and the environment [8]. Thus, when the ambient humidity is high, there is a reduction in the rate at which sweat is evaporated. Second, horses have a large body volume-to¬ skin surface ratio, which results in a relatively small surface area from which evaporation can occur [6]. Finally, it has been shown in humans that there is competition for cardiac output between the skin and muscle during exercise whereby maintenance of cardiovascular function takes precedence over ther¬moregulatory function [12]. This results in less blood flow to the skin, and ultimately a slower rate of heat loss than would occur if skin blood flow were maintained during exercise [9]. It has recently been shown that nonspe¬cific inhibition of nitric oxide synthase reduces the sweating response and increases the body temperature of exercising horses [13]. These findings sug¬gest that nitric oxide may modulate the sweating response to exercise in horses. It was not determined whether this modulation was acting centrally or peripherally.
Histology of equine sweat glands
Histological evaluation of the horse sweat gland has been performed [14].They are classified as apocrine, and in normal horses are tubular, with thesecretory portion being coiled and _mbedded within the dermis. A straightand unbranched duct opens into a hair follicle adjacent to the skin surface(Fig. 1).Evans et al [14] described the secretory tubules of equine sweat glands ashaving two layers: an inner layer of cuboidal secretory epithelial cells, andan enveloping layer of myoepithelium. These myoepithelial cells are restingon a basal lamina [15] and surrounded by a layer of connective tissue and an outer sheath of fibrocytes [16]. Within this fibrocytic sheath are small blood vessels and nerve fibers [17]. Histochemical staining reveals the presence ofmonoamine oxidase in the nerve fibers suggesting adrenergic fiber innerva¬tion [17]. The secretory cells have cytoplasmic protusions that extend intothe lumen of the duct [16] suggesting an apocrine mode of secretion. Theapocrine mechanism of secretion is further supported by the observationthat the secretory cells do not contain glycogen [18].
Physiology of sweating in horses
Physiologic control of sweating ill horses is unique compared with other species. Horses have two mechanisms of control; humoral control via
Fig. I.
Dual physiologic control of sweating in horses.adrenergic agonists secreted from the adrenal medulla into the circulation, and nervous control via autonomic adrenergic nerves [6]. Work in donkeys indicated that the main component of equid sweat control is neural, with the humoral component becoming active during exercise. [19] (Fig. I). Initial studies suggested both cholinergic and adrenergic agonists induced sweating in horses [20], but later studies have concluded that equine sweat glands are insensitive to carbamylcholine and controlled only by adrenergic neuro-transmitters [21]. It has been demonstrated that stimulation of equine sweat glands occurs through P2-adrenergic receptor stimulation [22,23].Investigations with individual equine sweat glands in vitro demonstrated that cyclic adenosine monophosphate (cAMP) acts as a principal second-messenger when Pradrenoreceptors are stimulated [24]. Subsequent studies with equine sweat gland epithelial cell cultures have conclusively established that sweating in horses is regulated by P2-adrenoreceptors and mediated by cAMP and possibly intracellular free Ca that mediate the effects of _ragonists involve occupation of the receptor bythe agonist, resulting in a conformational change in the ex-subunit of thestimulatory G protein. This protein is involved in the activation of adenylatecyclase, which catalyzes the formation of cAMP. Protein kinase A is thenformed and produces the subsequent phosphorylation of cellular proteinand altered cellular response [26] (Fig. 2). The autocrine role played by pyr¬imidine and purine nucleotide receptor stimulation in the control of sweat¬ing in horses remains to be determined [27].Potential mechanisms of anhidrosisAt present, the mechanisms of anhidrosis are unknown. Potential patho¬logic mechanisms can be classified as either a decreased stimulation of thesweat gland or a lack of response of the gland to stimulation.Central nervous system and nervous control
The Central nervous system (CNS), via the hypothalamus, provides con¬trol over both the humoral and neural mechanisms of anhidrosis [28]. Heatstroke is a real possibility in thermally stressed animals; temps of above108°F have been shown to cause CNS dysfunction in dogs [29]. Muscle tem¬peratures of up to 111°F have been recorded after intense exercise in horses, thereby illustrating the potential risk for CNS damage in these animals [7]
Receptor exposure to agonist. 0 G protein uncoupling and activation 01 adenylc He cyclase CD Formation 01 cAMP and protein kinase A catalysed by i'lcfenylilW
cyclase and subsequent phosphorylation of cellular proteins.
However, despite the possibility of CNS dysfunction occuring when bodylemperat_res are severely elevated, it is unlikely that this is a factor in anhi¬drosis as the syndrome is reversible [2], and horses develop the conditionwithout having developed such high temperatures.Although it has been shown that equine sweat glands are innervated! 14, 16], denervated horse skin retains the ability to produce sweat duringexercise via humoral stimulation [30]. Additionally, sweat gland innervation of anhidrotic horses has been reported to be normal. with no evidence ofaxonal degeneration [14]. These findings, coupled with the reversible natureof anhidrosis, make denervation an unlikely cause of anhidrosis. gland [32]. As such, duct obstruction is not considered to be a likely cause of anhidrosis [14,32].
The sweat glands of anhidrotic horses have been examined histologically after having undergone a period of thermal stress, and then again after 6 weeks in a controlled, cool environment [32]. Glandular profiles after ther¬mal stress were characterized by the degree of thinning or flattening and damage to the secretory cells. This may provide a means to predict the severity of anhidrosis and the prognosis for recovery, and to provide criteria for future management [32]. It can be concluded that cellular degeneration is a result, and not a cause, of anhidrosis [14,32].
Adrenal function
It has been hypothesized that decreased production of epinephrine by the adrenal medulla may be a cause of anhidrosis [20]. However, it has been reported that anhidrotic horses have higher circulating concentrations of epinephrine when compared with healthy horses [31]. Also, adrenomedullary denervated donkeys retain the ability to sweat in response to thermal stimulation [19]. Therefore, decreased production of epinephrine by the adre¬nal glands is an unlikely cause of anhidrosis. Desensitization or downregulation of receptors.
Heat stress may result in higher than normal concentrations of circulat¬ing epinephrine. Plasma taken from horses at rest showed significantly high¬er levels of epinephrine in anhidrotic horses compared with unaffected horses [31]. Catecholamines participate as _ragonists in both humoral and neural stimulation of sweating, and could potentially overstimulate _r receptors. Langley and Bennett described a decreased sensitivity to adrena¬line that occurred when they injected horses with adrenaline and then exercised them several hours later [33]. A corroborative study by Evans et al indicated that as a result of intravenous epinephrine administration, parti¬ally anhidrotic horses ceased sweating for 2 weeks [2]. A similar pheno¬menon, described as "persistent desensitization" of _2-adrenoreceptors, has been produced by incubating cultured equine sweat gland epithelial cells in a solution containing adrenaline [34]. This decreased sensitivity of _radreno¬receptors had an early and a late phase and resensitization of the Pr adrenoreceptors occurred slowly (t1/2 = 6.3 hours). The cause of this decreased sensitivity to adrenaline was not fully determined. However, it was shown that increased phosphodiesterase activity may have been contri¬buting to the late phase desensitivity. Both the in vivo and in vitro pheno¬mena described above document the fact that P2-adrenoreceptors in horse sweat glands are subject to decreased sensitivity following intense stimula¬tion. Further studies will be needed to determine the molecular basis for this "persistent desensitization" of P2-adrenoreceptors in equine sweat glands.In other species, overstimulation of _rreceptors can cause a diminished function of the receptors [35]. This can result in a marked reduction in the response of the receptors to further stimulation with a variable period of unresponsiveness. Historically, this phenomenon was described as desensiti¬zation or downregulation, but recent studies have shown that desensitiza¬tion is a separate entity from downregulation [36].Desensitization is a phosphorylation-dependant rapid uncoupling of the _rreceptor from the G protein. For resensitization to occur, sequestration of the receptor away from the normal site on the cell surface to another site within the cell must take place. Resensitization of the receptor is a slower
Sweat gland perfusion
An adequate vascular supply is important for umoral stimulation ofsweating. Electron microscopic examinations of blood vessels from anhi¬drotic horses demonstrated these structures to be normal [16]. Therefore,a structural vascular impairment does not appear to be a contributing fac¬tor. However, a dynamic impaired dermal perfusion can occur during in¬tense exercise when fluid loss and maintenance of cardiovascular function results in less blood flow to the skin [12].
Sweat gland histopathology
The ultrastructure of sweat glands from anhidrotic horses housed in hothumid conditions has been reported to be abnormal [16]. Reported abnor¬malities included thickened basal lamina, evidence of poor myoepithelialcontraction, fibrocytes with dilated endoplasmic reticulum and vacuolation,and thickened connective tissues. The secretory cells had a marked reductionof vesicles with increased numbers of mitochondria and less rough endoplas¬mic reticulum. The luminal microvilli were often absent, and the cells hadbecome flattened; in some cases, secretory granules were replaced by myo¬epithelium. Cellular debris was often present within the lumen of the duct,and in some cases the lumen was fully obstructed [I 4J. Duct obstruction hasbeen speculated to be a response to prolonged stress and failure of secretion,, and may provide a mechanism of defense. against microbes invading the process than the uncoupling mechanism of desensitization [36], and may be part of the normal mechanism of receptor turnover within cells.
Downregulation is an actual decrease in the total number of receptors in the cellular pool of receptors or a lower receptor density [36]. This is a slow process, and is a long-term mechanism that may involve altered receptor protein synthesis or altered receptor protein degradation. Downregulation has been shown to be accompanied by a decrease in _-adrenergic receptor messenger RNA concentrations [36].
Thyroid hormones
Thyroid hormones are known to have modulating effects on adrenergic receptors [35]. Tissues are more responsive to _-adrenergic catecholamines when thyroid hormone concentrations are elevated, and conversely, when hypothyroidism occurs, they are less responsive [37]. In himans, symptoms of hyperthyroidism suggest increased sympathetic drive or increased plasma concentrations of catecholamines [35]. It has also been shown that there is a decreased density of _-adrenergic receptors in hypothyroid animals, decreased receptor coupling to the adenylate cyclase system, and ultimately receptor function is minimized [38]. The role played by thyroid hormones in the pathophysiology of anhidrosis is equivocal. In horses, some of the sec¬ondary clinical signs of decreased thyroid function are similar to those of anhidrosis [5]; however, it has been reported that thyroidectomized horses appear to sweat normally [39]. It has also been reported that there is no stat¬istical difference in T 3 and T 4 plasma concentrations between normal and anhidrotic horses [3]. However, therapy with iodinated casein, a thyroid hormone precursor, has some reports of success [40]. This latter finding allows postulation that there may be a role played by thyroid hormones.
Electrolyte abnormalities
The effect of electrolyte losses incurred during exercise and long-term exposure to a hot humid climate is often thought to be involved in anhidro¬sis: one common therapeutic approach is oral electrolyte supplementation [3]. Even though significant quantities of electrolytes, including potassium and calcium, are lost in sweat [41], statistically significant electrolyte abnor¬malities have not been reported for horse with anhidrosis.
Experimental depletion of extracellular and presumably intracellular Ca ++ in vitro decreased the sweat response, indicating that sweat secretion may be dependent upon concentrations of intracellular calcium [24]. How¬ever, hypocalcemia has not been reported as a cause of anhidrosis. Low potassium intake in ponies resulted in a more rapid onset of fatigue during treadmill exercise and decreased sweat production [42]. Although these ponies were hypokalemic, studies have shown that anhidrotic horses have , normal serum potassium concentrations [3]. However, as potassium is maiply intracellular, total body potassium may be depleted, but undetected, and this would help to explain anecdotal reports that some anhidrotic horses respond to oral potassium supplementation.
Diagnosis of anhidrosis
Diagnosis of anhidrosis can be tentatively made based on clinical signs and performance. It should be emphasized that, based on the development of increased respiratory effort and hyperthermia, anhidrotic horses are com¬monly presented to veterinary practitioners for diagnosis and treatment of respiratory disease. However, a semiquantitative test to evaluate sweating by induction of the sweat response, using dilute concentrations of epineph¬rine injected intradermally, has been developed, and will provide a more definitive diagnosis [43]. However, epinephrine is not completely suitable for such a diagnostic test because it has both _- and a.-adrenergic receptor ago¬nist properties, and therefore, may cause leukotrichia at the injection sites. Salbutamol sulfate, a specific _ragonist, has been described for use in a semiquantitative test for anhidrosis in Thoroughbred horses [44]. A control of sterile water and six dilutions of salbutamol, from 10-3 w\v to IO'-R w\v, were injected intradermally. The results were read 20 minutes later. Horses with long-standing anhidrosis did not sweat at any of the dilutions. Normal horses sweated in response to the 10-8 w\v dilution, and partially anhidrotic horses responded with dilutions between 10-4 w\v and 10-6 w\v. An unre¬ported, semiquantitative test using terbutaline sulfate, another specific _2-adrenergic receptor agonist, is also diagnostic (R.E. Beadle, personal com¬munication, Louisiana State University, Baton Rouge, LA). The protocol and results are similar to that of the test using salbutamol, except a physiol¬ogic saline solution control is used (Figs. 3,4 and 5).
Treating anhidrosis
Because there are no known proven treatments for anhidrosis, all of the therapies described for this condition are anecdotal. Treatment of anhidrosis can be categorized into management changes or medical therapy. A combi¬nation of both categories is usually necessary for any success in the manage¬ment of this condition.
Management changes
The most reliable treatment for anhidrosis is environmental control. This involves management changes directed at removing anhidrotic horses from hot, humid climates and moving them to a cooler, drier environment. Ten to 30 days in such an environment for affected horses has been reported to relieve the signs [2]. In lieu of moving the affected animal, other management changes that are directed to providing a cooler environment may be of some benefit. These changes may include placing the animal in an air-conditioned stall. The use of misting fans and cooling the roof of the barn by running
Fig. 3. Response of normal horse toa semiquantitative test used to diagnose anhidrosis.
Fig. 4. A partial sweater. There is only a minimal response to the intradermal injections of a specific _radrenergic agonist.
Fig. 5. An anhidrotic horse: there is a complete lack of response to the specific _2-adrenergic agoni_t. water on it will help maintain a cooler environment. Exercising the horse during the coolest part of the day is another adjustment that will help man¬age the disease.
Medical therapies
Electrolyte supplementation Horses with anhidrosis have reported serum electrolyte values within nor¬mal limits [3]. However, hypokalemia is often suspected in the etiology of anhidrosis [39]. Some practitioners report some success in supplementing with 60 g of KCI or lite salt in the feed. Intubation over several days with two packs of commercial electrolyte replacement product (Enterolyte H.E., Pfizer) has also been used with some success.
Dietary supplements
A nutritional feed supplement that contains L-tyrosine, ascorbic acid, and niacin is commercially available (One AC, MP Co., Phoenix, AZ). Tyrosine is potentially involved in the resensitization of sequestered _rreceptors [45], and is a precusor for the formation of dopamine and thus catecholamines. However, plasma tyrosine levels are not decreased in anhi¬drotic horses [46].
Anecdotal reports among practitioners indicate a success rate of 30-80% using One AC, with the best results seen in moderately affected horses and by placing previously affected animals on the product prior to the beginning of the anhidrotic season. Best results are reported if strenuous training or work is reduced for approximately 3 weeks when started on the supplement. It should be noted that a lessening of the intensity of training or work alone has been reported to relieve the clinical signs of anhidrosis.
Methyl dopa
Using drugs to decrease sympathetic drive would seem to be logical in treating horses with anhidrosis. Methyl dopa has been used by some practi¬tioners with reported success. An initial dosage of 3000 mg once daily was used increasing to 4000 mg once daily if no positive response in 3-4 days.
In humans, methyl dopa decreases sympathetic outflow from the CNS and is associated with decreased tissue concentrations of norepinephrine and epinephrine [47]. When an anhidrotic horse is treated with this drug, the concentration of epinephrine at the _2-adrenergic receptor site would be expected to decrease, which may allow receptor resensitization. Despite anecdotal reports of success there are no controlled studies of the efficiency of this agent in anhidrotic horses.
Thyroid supplementation
Administering iodinated casein orally at 10-15 g per day for 4 to 8 days has been reported to be beneficial in the literature [40]. Practitioners havereported success supplementing with levo-thyroxine (THYRO-L, Vetamix, ShenandQah, IA) at a dose of 0.5-3.0 mg per 100 Ib once a day. Hypothyroidism may exhibit similar clinical signs as anhidrosis, but there has been no documentation of changes in T 3 or T 4 levels in horses living in tropical or semitropical environments or with anhidrosis. Care should be taken when treating a horse with levo-thyroxine supplementation, as the resultant increased metabolic rate could be harmful with the completely anhidrotic horse overheating when exercised in extremely hot and humid weather.
Summary
The molecular basis of the pathophysiology of anhidrosis is still not well understood. Therefore, treatments are more often based on clinical impressions than on scientific fact. Treatment options for this condition will improve only when more is known about the molecular events that cause an-hidrosis, especially as they relate to _2-receptor dysfunction and stimulus¬secretion coupling in the sweat glands of affected horses. Although this additional information is being attained, sound environmental management will continue to be a very important aspect of the treatment of horses affected with anhidrosis.
Clenbuterol
There have been anecdotal reports that clenbuterol is effective in causing sweating in some anhidrotic horses. Clenbuterol is a _2-adrenergic agonist, and mild sweating is a recognized side effect of clenbuterol administration for respiratory signs especially at the higher dosage. Its effect is probably mutifac¬eted; both direct stimulation of the receptors on the sweat glands and increased peripheral blood flow. This increased blood flow could help cool the horse. The reported dosages ranged from 5-10 mlllOOO lbs of a 72.5 mcg/ml solution orally twice a day.
The authors do not recommend the use of clenbuterol, as a prior report [43] indicates that stimulation of the sweat glands of anhidrotic horses with an exogenous _ragonist results in enhanced prolonged desensitization.
Alternative therapies
There have been anecdotal reports of return to sweating following acupuncture. This response has been reported to last from a few days to several weeks. There have also been reports of success using homeopathic substances, that is, sulphur and lycopodium in combination.
Future therapies
In humans, it has been shown that glucocorticoids increase the _rrecep¬tor gene in several cell types, and that glucocorticoids may prevent desensi¬tization and restore downregulated receptors [48,49]. Other drugs such as nedocromil sodium and ketotifen have been reported to reduce the down¬. regulation of _2-receptors as well [50,51].
References
One practitioner has reported response of anhidrotic horses to rubeolla virus immunomodulation while treating muscle problems (R.V.I., Eudae¬monic Corporation, Omaha, NE). Lay persons have reported success by feeding dark beer daily.
(1] Wright TWW, Tull TC. A preliminary report of an investigation of a condition known as "dry coat" in horses. Vet J 1925;81:235.
[2] Evans CL, Smith DFG, Ross KA, et al. Physiological factors in the condition of "dry coat in horses. Vet Rec 1957;69:l.
[3] Mayhew IG, Ferguson HO. Clinical, clinicopathologic, and epidemiologic features of anhidrosis in central Florida Thoroughbred horses. J Vet Intern Med 1987;1:136.
[4] Warner AE, Mayhew IG. Equine anhidrosis: a survey of affected horses in Florida. ] AmVet Med Assoc 1982;180:627.
[5] Currie AK, Seager SWJ. Anhidrosis. In: Proceedings AAEP Annual Meeting; Dallas, TX.Nov 28-Dec I, 1976, p. 249.
[6] Hodgson DR, McCutcheon LJ, Byrd SK, et al. Dissipation of metabolic heat in the horseduring exercise. J Appl Physiol 1993;74: 116l.
[7] Robertshaw D. The evolution of thermoregulatory sweating in man and animals. Int JBiometeorol 1971; 15:263.
[8] Geor RJ, McCutcheon LJ. Thermoregulation and clinical disorders associated withexercise and heat stress. Compend Contin Educ Pract Vet 1996;18:436.
[9] Ingjer F, Stromme SB. Effects of active, passive or no warm up on the physiologicalresponse to heavy exercise. Eur J Appl PhysioI1979;40:273.
[10] Nadel ER. Temperature regulation and prolonged exercise. Perspectives in exercise scienceand sports medicine. Carmel (IN): Benchmark Press; 1988. p. 125.[II] Carlson GP. Thermoregulation and fluid balance in the exercising horse. In: Snow DH,Persson SGB, Rose RJ. editors. Equine exercise physiology. Cambridge. UK: GrantaPublications; 1983. p. 291.
[12] Nadel ER, Cafarelli E, Roberts MF, et al. Circulatory regulation during exercise indifferent ambient temperatures. J Appl Physiol 1979;46:430.
[13] Mills PC, Marlin DJ, Scott CM. et al. Nitric oxide and thermoregulation during exercise inthe horse. J Appl Physiol 1997;82: 1035.
[14] Evans CL, Nisbet AM, Ross KA. A histological study of the sweat glands of normal anddry coated horses. J Comp Pathol 1957;67:397.
[15] Bal SH. The skin. In: Swenson MJ. Reece WO, editors. Dukes' physiology of domesticanimals. Ithaca (NY): Cornell University Press; 1993. p. 622.
[16] Jenkinson OM, Montgomery I. Elder HY, et al. Ultrastructural variations in the sweatglands of anhidrotic horses. Equine Vet J 1985;17:287.
[17] Jenkinson DM, Blackburn PS. The distribution of nerves, monoamine oxidase and cholinesterase in the skin of the horse. Res Vet Sci 1968;9: 165.
[18] Sorensen VW, Prasad O. On the fine structure of horse sweat glands. Z Anat Entwickl. Oesch 1973;139:173.
[19] Robertshaw D. Taylor CR. Sweat gland function of the donkey (Equus asinus). J Physiol 1969:205:79.
[20] Eva'ns CL. Smith DFG. Sweating responses in the horse. Proc R Soc Lond Series Bioi Sci 1956;145:61.
[21] Johnson KG, Creed KE. Sweating in the intact horse and isolated perfused horse skin. Comp Biochem Physio1 1982:73:259.
[22] Bijman J, Quinton PM. Predominantly _-adrenergic control of equine sweating. Am J Physiol 1984;246:R349.
[23) Snow DH. Identification of the receptor involved in adrenaline mediated sweating in the horse. Res Vet Sci 1977;23:246.
[24] Bijman J. Quinton PM. Influence of calcium and cyclic nucleotides on beta-adrenergic sweat secretion in equine sweat glands. Am J Physiol 1984;247:CI0.
[25] Wilson SM. Pediani JD, Ko WHo et a!. Investigation of stimulus-secretion coupling in equine sweat gland epithelia using cell culture techniques. J Exp Bioi 1993; 183:279.
[26] Barnes P1. Beta-adrenergic receptors and their regulation. Am J Respir Crit Care Med 1995;152:838.
[27] Ko WH, Wilson SM. Wong PY. Purine and pyrimidine nucleotide receptors in the apical membranes of equine cultured epithelia. Br J Pharmacol 1997;121:150.
[28] Detweiler DK. Control mechanisms of the circulatory system. In: Swenson MJ, Reece WO, editors. Dukes' physiology of domestic animals. Ithaca (NY): Cornell University Press; 1993. p. 216.
[29) Brinnel H, Cabanac M, Hales JRS. Critical upper levels of body temperature, tissue thermosensitivity
and selective brain cooling in hyperthermia. In: Hales RJS, Richards DAB, editors. Heat stress: physical exertion and environment. Amsterdam, Holland: Elsevier Science Publications; 1987. p. 209.
[30) Robertshaw D. Neural and humoral control of apocrine glands. J Invest Dermatol 1974; 63:160.
[31) Beadle RE, Norwood GL, Brencick V A. Summertime plasma catecholamine concentra¬ tions in healthy and anhidrotic horses in Louisiana. Am J Vet Res 1982;43: 1446.
[32) Jenkinson DM, Loney C, Elder HY, et al. Effects of season and lower ambient temperature on the structure of the sweat glands in anhidrotic horses. Equine Vet J 1989;21:59.
[33] Langley IN. Bennett S. Action of pilocarpine, arecoline and adrenaline on sweating in the horse. J Physiol (Lond) 1923;57:Plxxi.
[34] Rakhit S, Murdoch R, Wilson SM. Persistent desensitisation of the beta 2 adrenoceptors expressed by cultured equine sweat gland epithelial cells. J Exp Bioi 1998;201(Pt 2):259. [35] Lefkowitz RJ, Caron MG, Stiles GL. Mechanisms of membrane-receptor regulation. Biochemical. physiological. and clinical insights derived from studies of the adrenergic receptors. N Engl J Med 1984:310: 1570. [36) Stiles GL. Structure and function of cardiovascular membranes, channels, and receptors. In: Schlant RC, Alexander RW, editors. Hurst's the heart. New York: McGraw-Hill Book Co.: 1994. p. 54.
[37] Bilezikian JP. Loeb IN, Gammon DE. The influence of hyperthyroidism and hypo¬ thyroidism on the _-adrenergic responsiveness of the turkey erythrocyte. J Clin Invest 1979;63: 184.
[38] Stiles GL. Stadel JM, De Lean A, et a!. Hypothyroidism modulates beta adrenergic receptor-adenylate cyclase interactions in rat reticulocytes. J Clin Invest 1981 ;68: 1450.
[39] Warner A, Mayhew IG. Equine anhidrosis: a review of pathophysiologic mechanisms. Vet Res Commun 1983;6:249.
[40] Maqsood M. Iodinated casein therapy for the non-sweating syndrome in horses. Vet Rec 1956;68:475.
[41] Carlson GP, Ocen PO. Composition of equine sweat following exercise in high environ¬ mental temperatures and in response to intravenous epinephrine administration. J Equine Med Surg 1979:3:27.
[42] Meyer H. Gurer C. Linder A. Effects of a low potassium diet on potassium metabolism, sweat production and sweat composition in horses.
In Proceedings of Equine Nutrition & Physiology Society Symposium; East Lansing, Ml. May 23 ...25. 1985. p. 130.
[43] Evans CL. Physiological mechanisms that underlie sweating in the horse. Br Vet J 1966: 122: 117.
[44] Guthrie AJ, Van den Berg JS, Killeen VM, et a!. Use of a semi-quantitative sweat test in thoroughbred horses. J S Afr Vet Assoc 1992;63:162.
[45] Barak LS, Tiberi M, Freedman NJ, et al. A highly conserved tyrosine residue in G protein¬ coupled receptors is required for agonist-mediated Pradrenergic receptoi' sequestration. J Bioi Chern 1994;269:2790.
[46] Lieb S, Bowker K, Lester G, et al. The effect of a nutrient supplement on the respiration, pulse, temperature, sweating and serum electrolyte and amino acid levels of anhidrotic horses. In: 14th Equine Nutrition & Physiology Society Symposium: Ontario, CA, January 19--25. 1995. p. 87.
[47] Rudd P, Blaschke TF. Antihypertensive agents and the drug therapy of hypertension. In:
Goodman and Gilman's: the pharmacological basis of therapeutics. 7th ed. New York:
Macmillian; 1985. p. 784.
[48) Barnes PJ. Molecular biology of receptors. Q J Med 1992;83:339. [49] Hui KK, Conolly ME, Tashkin DP. Reversal of human lymphocyte _-adrenoceptor desensitization by glucocorticoids. Clin Pharmacol Ther 1982;32:566.
[50] Bretz U, Martin U, Mazzoni L, et al. _-Adrenergic tachyphylaxis in the rat and its reversal and prevention by ketotifen. Em J Pharmacol 1983;86:321.
[51] Kioumis I, Ukena D, Barnes PJ. Effect of nedocromil sodium on down-regulation of pulmonary _-adrenoceptors. Clin Sci (Coleh) 1989;76:599.
See & Print the Studies:



